Copyright The Boston Globe
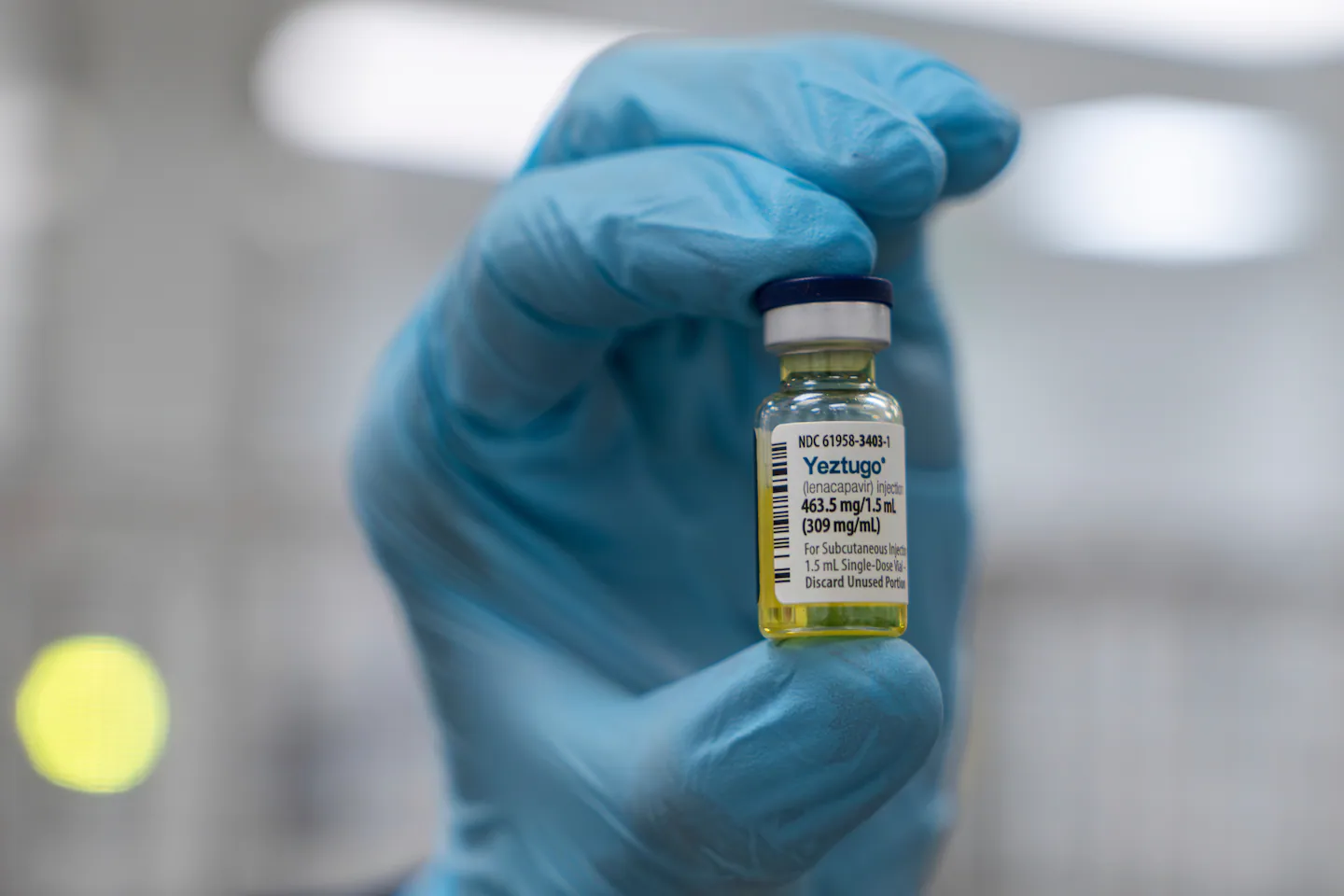
The life expectancy for HIV positive persons is now similar to the general population. These advances stem from decades of research to develop medications that have revolutionized HIV treatment into a single daily pill. We also know that treatment is prevention. HIV positive persons who take their medications regularly and have a suppressed viral load do not transmit HIV to others. Moreover, in 2012, the FDA approved a daily oral medication called pre-exposure prophylaxis, or PrEP. When people without HIV take PrEP regularly, their HIV risks are reduced to nearly zero. In other words, with as little as one daily pill, most HIV infections can be both treated and prevented. However, some of the populations most likely to need PrEP are also likely to have trouble keeping up with a daily pill regimen. Adherence can be especially challenging for younger people, people with mental health conditions, or people who use drugs. There is a solution for this. New PrEP formulations known as long-acting agents reduce the burden of taking pills every day and can help people stay HIV-negative. Lenacapavir is a new injectable medication, given twice per year, approved by the FDA in June 2025. The Centers for Disease Control and Prevention released new guidelines for lenacapavir use last month. There is another injectable medication called cabotegravir, which is administered every two months and was approved by the FDA in 2021. Although the Trump administration has terminated hundreds of millions in research grants focused on HIV prevention, the NIH strategic plan released in August 2025 doubles down on HIV prevention and calls for new focus on scaling long-acting PrEP and treatment agents across the country. This new commitment aligns with President Trump’s 2019 commitment and National Plan to End the HIV epidemic. The Supreme Court also recently upheld the Affordable Care Act, which requires insurance companies to pay for preventive health services, and the US Preventive Services Task Force recommends PrEP be covered with no out-of-pocket expenses. In spite of the task force guidelines, many patients nationwide continue to experience exorbitant copayments and deductibles for PrEP medications. We agree with the NIH that long-acting agents are a critical component of any national strategy to end the HIV epidemic. PrEP should also be covered by insurance plans in accordance with the Affordable Care Act guidelines. Our decade of research on PrEP demonstrates that reducing barriers like copayments and deductibles would enhance many patients’ ability to stay in HIV-prevention services, and ultimately to remain HIV negative. Although the federal Ryan White program is the payer of last resort for HIV-positive persons, there is no such federal program for HIV-negative persons, and many people still can’t afford PrEP. In 2023 in Rhode Island, several of our patients at Open Door Health and the Rhode Island Public Health Institute contracted HIV when they stopped taking PrEP because of their high deductibles and copayments. The Rhode Island Public Health Institute then led an advocacy coalition to expand access to PrEP statewide. The result: new state laws require insurance companies to cover PrEP and eliminate all copayments and deductibles, allow pharmacists to prescribe PrEP, and eliminate prior authorizations and “step therapies,” which require doctors to prescribe cheapest medicines first. However, it is very hard to access lenacapavir in Rhode Island and elsewhere across the United States. We have trouble getting this life-saving medication at affordable costs for many of our patients who want to take it. Medicare and the Veterans Administration have already added lenacapavir to their formularies, recognizing it as a cost-effective strategy for reducing HIV transmission. Despite these significant government actions to make this medication widely accessible, CVS Health, the largest pharmacy benefit manager in the country, headquartered in our home state of Rhode Island, has not added lenacapavir to its formularies as a no-cost preventative service. This has huge implications for impeding access to this medication nationwide, as CVS has outsized market share for controlling national medication supply. CVS is one of the top three US pharmacy benefit managers, which together control 70 percent of specialty drug prescriptions nationwide. Many people who could benefit may not have access to these treatments nationwide because of CVS’ lenacapavir policy. Insurers will also face challenges in complying with PrEP laws nationwide that mandate coverage of injectable PrEP formulations, like in Rhode Island. We finally have the technology, infrastructure, and the political will to end the country’s HIV epidemic. But access to PrEP medications remains incredibly uneven, and too many people still experience exorbitant out-of-pocket costs for medications. CVS needs to expand access to life-saving medication for the hundreds of thousands of people who need injectable PrEP. Their policies will affect our ability to prevent our patients from contracting HIV.