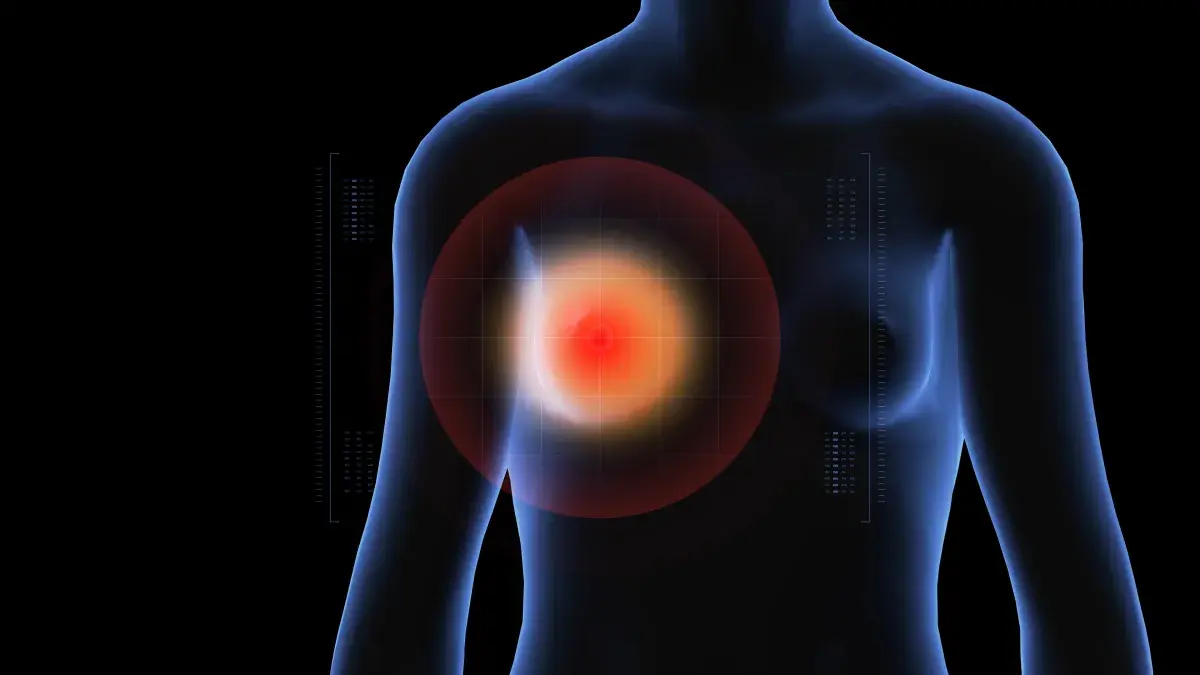
When Candace Smith first discovered a painful lump in her breast at age 37, she never imagined it would lead to rare diagnosis.
Now 52, the North Carolina woman told Newsweek about her experience with granulomatous mastitis—a benign but chronic inflammatory breast disease estimated to affect roughly 2.4 in every 100,000 women. However, experts believe the real number is likely far higher, as the condition is frequently misdiagnosed.
The cause of this condition is unknown, but one study points out that it can start when milk gets trapped in the breast—often during or after pregnancy or breastfeeding—because of hormonal changes. Or certain bacteria, such as the naturally occurring corynebacterium, may worsen the reaction, leading to small pockets of infection and the formation of lumps called granulomas.
Smith told Newsweek: “I believe I contracted granulomatous mastitis through dirt, as I was gardening.”
Newsweek also spoke to Dr. Kelly McLean, a surgical oncologist, who said: “The misunderstanding of the origin of granulomatous mastitis likely stems from the fact that the most-common bacterium in granulomatous mastitis is corynebacterium.”
These types of bacteria are very common. They naturally live in places like soil and are also often found on the skin and in the moist linings of the nose, mouth and other body surfaces of both people and animals.
McLean, who works at The Christ Hospital in Cincinnati, Ohio, said that the bacteria thrive in fatty areas. Because breast tissue is mostly fat, it provides the perfect place for them to grow.
However, corynebacterium is hard to detect with the usual lab test, which involves growing bacteria on a plate. When they don’t grow, it can appear as if there is no infection at all.
Recognizing the Symptoms
Granulomatous mastitis is a chronic, unpredictable breast inflammation with flare-ups similar to autoimmune diseases such as rheumatoid arthritis, lupus or inflammatory thyroid disorders. In these cases, the body’s immune cells mistakenly attack breast tissue instead of fighting infection.
The warning signs include:
Breast Mass: Inflammatory tissue (phlegmon) that can become large and feel like a tumor.
Skin Changes: Dark red, violet or brownish-red patches on the skin.
Open Wounds: One or more lesions that may drain thin, watery, mucoid or bloody fluid.
Pain: Localized breast pain varying in intensity.
A Painful Journey
“I was diagnosed in 2010 when I presented with a fast-growing painful lump in my breast,” Smith said, adding that medics weren’t familiar with the condition, making it “very scary.”
“The doctors had no knowledge of how to treat it properly. I was put on steroids, which did make me feel a bit better, but they have so many side effects, and it is not a reliable form of treatment that we have seen.”
McLean added: “Because of the bacterium’s structure, it can be difficult for the body to kill. Instead, the body attempts to wall the bacteria off from healthy tissue, forming the characteristic granulomas that are seen under the microscope and that give the disease its name. What was once thought to be a sterile mass of inflammatory reaction is likely a collection of micro-abscesses.
“In the past, the disease appeared to spread when surgical interventions were applied. This was thought to be due to further stimulation of the immune response. When the area is surgically removed or biopsied, the infection spreads, perpetuating the disease.”
‘It Was Utterly Debilitating’
Smith said: “When I had granulomatous mastitis, it was very overwhelming. There was excruciating pain from an open surgical wound from biopsy that needed to be cleaned and packed.
“Most daily movement caused pain, and taking care of a child during this time added even more opportunity for random bumps that could make you cry out in pain. I developed severe lethargy, which made it extremely difficult to do daily tasks, let alone take care of a child.
“I vividly remember sitting on the floor of my shower because I didn’t have the energy to stand. It was utterly debilitating. I don’t think you can effectively relay that type of experience to someone who has not felt it.
“Doctors just can’t seem to understand what this really does to our bodies, let alone the toll it takes on our womanhood with the disfigurement that can occur.”
Struggling for Diagnosis and Support
Smith, who now runs an online support group, said: “I believe most cases of granulomatous mastitis can be treated effectively, but the problem we see is getting a diagnosis.
“This unfortunately leads to so many members who are left to deal with granulomatous mastitis and suffer until it (hopefully) goes away, which can be years.
“Unfortunately, it puts women in danger due to the infection and extensive inflammation that it causes. This, in turn, can put us at higher risk for sepsis and cancer, both of which we have seen in the group.”
Breast Cancer Concerns
Newsweek also spoke to Lara Shelrud, 46, who was diagnosed in April 2021 after doctors initially suspected breast cancer.
The physiotherapist from Alberta, Canada, said: “My initial symptoms were pain and a palpable lump in one breast. The lump developed seemingly overnight.
“Initially, every doctor I saw was very concerned that I had breast cancer. When my first biopsy came back as noncancerous, everyone was confused.”
McLean told Newsweek that the inflammation caused by granulomatous mastitis can make it harder to spot breast cancer. Because the breast tissue is already swollen and irritated, imaging tests such as mammograms or ultrasounds are more difficult to read, which means that, if breast cancer is present at the same time, it could go unnoticed. And the initial presentation of granulomatous mastitis may appear to be a breast cancer.
After two biopsies, an MRI and several tests for tuberculosis, Shelrud was diagnosed with granulomatous mastitis.
“My infectious disease doctor said this bacterium is ‘just around in the environment’. Some people are affected by it, and some are not.”
The initial diagnosis brought frequent medical visits and tests for Shelrud, including one emergency room trip for a suspected biopsy-related infection.
Recovery required five months off work due to surgery, followed by two months of IV antibiotics through a peripherally inserted central catheter (PICC line) and ongoing wound care.
Because of a physical job and a 10-pound lifting limit, normal activities were restricted, significantly limiting both household tasks and the ability to care for her children.