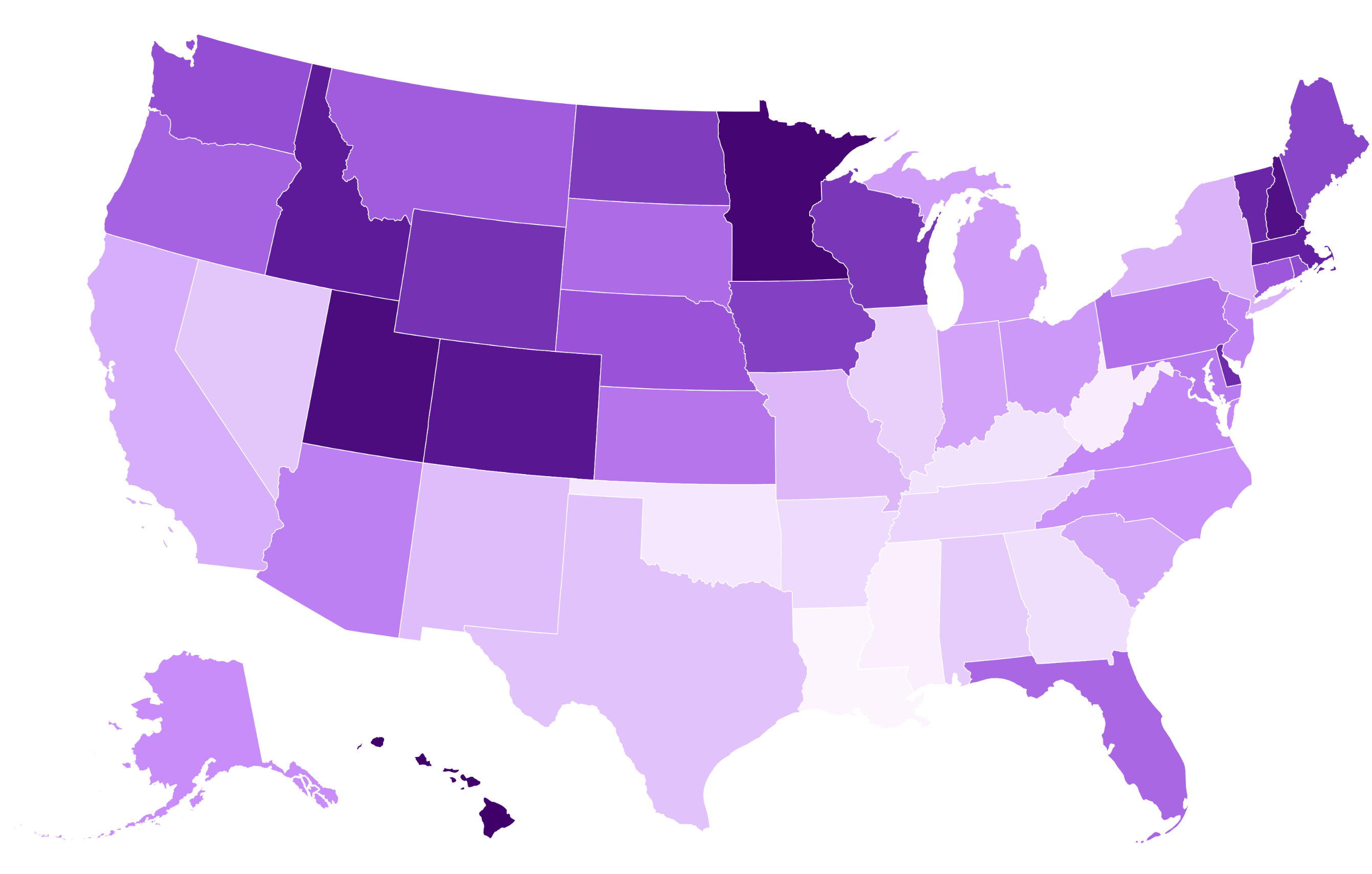
The health and well-being of America’s growing senior population differs significantly from state to state, and a new analysis has revealed which are leading—and falling behind—when it comes to caring for the elderly.
RetirementLiving.com, a website that provides information and planning tools for those in or entering retirement, graded each state across the nation on a number of metrics, before ranking them based on their overall senior care.
Why It Matters
Senior care or “eldercare” has garnered increased attention in the U.S. in recent years, as America’s aging population makes existing issues in the wider health care ecosystem—costs, access, labor shortfalls—more transparent. As noted in the study by Retirement Living, such issues affect not only the elderly but also caregivers, families and the health care sectors in each state.
What To Know
Drawing on the most recent available data from government sources and health care nonprofits, Retirement Living evaluated each state in three main categories, using these to come up with their overall ranking. States were assessed based on health care accessibility for senior citizens—factoring in things like nursing home quality and preventable hospitalizations—social factors such as poverty and senior isolation, as well as aspects of the state’s physical environment that could impact health.
Hawaii ranked top in the nation for senior care thanks to a strong performance across all three categories. Retirement Living cited the high quality of nursing homes, low rates of preventable hospitalizations as well as favorable environmental and social factors that helped make the Aloha State the “gold standard” for eldercare in the U.S.
Following Hawaii is Minnesota, thanks in part to strong health care accessibility and low levels of food insecurity in the state. Utah ranks third, benefiting from affordability, low social isolation among seniors and an environment described as “conducive to healthy senior living.”
The remainder of the states in Retirement Living’s top ten are:
4. New Hampshire
5. Colorado
6. Idaho
7. Massachusetts
8. Vermont
9. Delaware
10. Wyoming
Louisiana, meanwhile, ranks as the worst state in the U.S. for senior care according to Retirement Living’s analysis. As well as low-quality nursing facilities and high rates of preventable hospitalizations, researchers noted that the state’s health care system has “some of the worst health outcomes in the country,” a fact acknowledged in other analyses.
“The physical environment is another drawback for seniors in Louisiana. Air quality falls below average, while access to parks is limited throughout the state,” researchers wrote. “Louisiana also has the second-worst drinking water in the U.S., which poses a significant health and safety risk for all residents, but particularly for seniors.”
With the highest rates of both senior poverty and social isolation in the U.S., Mississippi comes in second last place, followed by West Virginia, the state with the worst senior health care access and the most preventable hospitalizations in the nation.
The remaining states in the bottom ten are:
47. Oklahoma
46. Kentucky
45. Georgia
44. Arkansas
43. Tennessee
42. Illinoi
41. Alabama
40. Nevada
Newsweek contacted the departments of health for Hawaii and Louisiana on Friday for comment.
What People Are Saying
Jailyn Rodriguez, who led the analysis for Retirement Living’s study, told Newsweek: “The Retirement Living Research Team found that states in the Northeast and Upper Midwest generally come out ahead because they put more resources into senior services, have higher-quality nursing homes, and a stronger base of geriatric specialists.
“On the flip side, many Southern states face steeper challenges—things like higher rates of senior poverty and food insecurity, plus fewer healthcare providers. Those factors combined often translate into worse outcomes, including more preventable hospitalizations.”
What Happens Next?
According to Rodriguez, there are signs of “both progress and ongoing challenges” in American senior care.
“Access to geriatric clinicians has improved since 2024, now at nearly 40 per 100,000 seniors, and hospice use has edged up slightly to roughly 47 percent of Medicare decedents,” she told Newsweek. “Community support spending is holding steady, showing continued investment in programs that help older adults stay connected and supported.”
However, she added that preventable hospitalizations have risen slightly between 2024 and 2025, with senior poverty and nursing home quality also worsening.