By Courtenay Harris Bond
Copyright phillyvoice
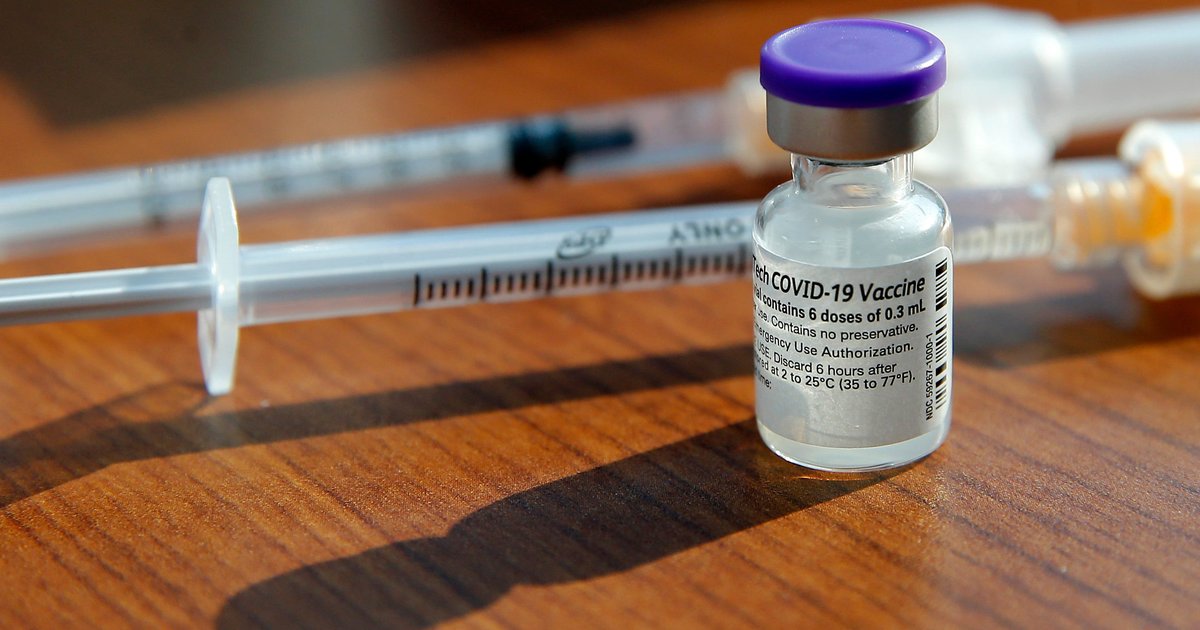
Health insurers will cover the cost of COVID-19, flu and other vaccines through 2026 regardless of what an advisory committee to the Centers for Disease Control and Prevention recommends.
The Advisory Committee on Immunization Practices is set to review and make recommendations Thursday on the COVID-19, hepatitis B, varicella and measles, mumps and rubella vaccines, according to the panel’s agenda. Health and Human Services Secretary Robert F. Kennedy fired the entire 17-member panel in June and replaced them with allies and vaccine skeptics. That, coupled with the Food and Drug Administration’s stiffer COVID-19 vaccine guidelines, had created confusion about whether people would have access to the shots — and whether insurers would cover them.
MORE: Blueberries help boost babies’ immune systems and gut health, study shows
On Tuesday, AHIP, a trade organization representing health insurers, said its members will cover all immunizations recommended by the ACIP — the CDC advisory panel — as of Sept. 1, clearing up some of the confusion. Insurers are required to cover any vaccines recommended by the panel.
“It’s a very positive step that the insurance industry is calling this travesty for what it is, rather than accepting the current A.C.I.P. will be able to protect the health of the patients they are responsible for,” Dr. Richard Besser, chief executive of the Robert Wood Johnson Foundation and a former acting director of the C.D.C., told the New York Times.
The new FDA guidelines advised COVID-19 shots only for people 65 and older and people with underlying health conditions that put them at high risk of severe COVID. This was a shift from previous guidelines, which recommended nearly everyone 6 and older get vaccinated.
After the FDA changed its COVID-19 vaccine guidelines, many states, including Pennsylvania and New Jersey, issued orders allowing pharmacists to vaccinate people against COVID without requiring prescriptions.
But questions remained about whether insurance companies would pay for the vaccines given to people who did not meet the FDA’s new eligibility guidelines.
“Independence Blue Cross continues to provide coverage for routine preventive vaccines at no cost to members,” the insurer, the largest in the Philadelphia region, said in a statement Thursday. “This coverage is in line with the preventive care service requirements outlined in the Affordable Care Act. It is also guided by recommendations from the Advisory Committee on Immunization Practices, as well as by professional society guidelines and evidence of vaccine safety and effectiveness.”
A recent analysis by NBC News found that childhood vaccination rates dropped in nearly 80% of U.S. counties since 2019.
“As childhood vaccination rates fall, we’ll see more diseases like measles,” Dr. Sean O’Leary, an infectious diseases expert with the American Academy of Pediatrics, told NBC News. “And we’ll see more children die — tragically — from diseases that are essentially entirely preventable.”