By Ashfaq Yusufzai
Copyright dawn
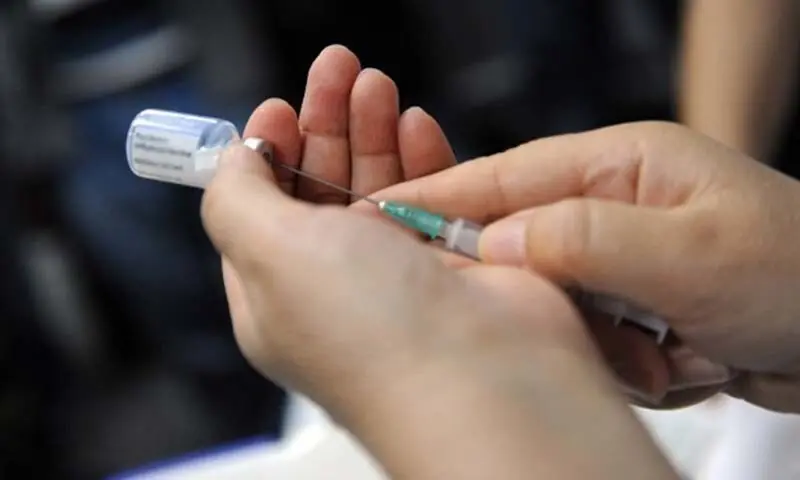
PESHAWAR: Severe shortage of trained and qualified anaesthetists has been putting the lives of patients at risk in private and public hospitals as doctors stay away from doing specialisation in this field of medical science owing to lack of incentives, according to a study.
Quackery in anaesthesia has been the main reason of high mortality, disabilities, cardiac arrests, brain damage and preventable deaths, says the study conducted by Khyber Pakhtunkhwa Society of Anaesthesia (KPSA).
It has suggested ban on unsupervised administration of anaesthesia to patients by technicians and deployment of qualified anaesthetists, especially in peripheral hospitals, to safeguard patients’ lives. Additionally, incentives and allowances should be announced to attract specialists and do away with quackery in this critical area, it adds.
The society wants Health Care Commission (HCC) to take action against the hospitals operating without qualified anaesthesia doctors, technicians and nurses. The government should remove from its panel of Sehat Card Plus (SCP), the free healthcare insurance initiative, such hospitals to save patients from complications, it adds.
Action sought against health facilities working without qualified specialists
The study shows that less than one per cent surgeries are performed under the supervision of anaesthesia specialists in Khyber Pakhtunkhwa.
It says that anaesthesia is a state of controlled reversible depression of central nervous system, loss of pain perception and immobility that is sufficient to permit the performance of surgery or other painful procedures in middle income countries like Pakistan where anaesthesia-related deaths after or during surgical procedures are one in 300 in comparison to one in 10,000 in developed countries.
The study says that anaesthesia is used in surgical or other procedure to relieve pain during surgery to keep patients asleep or pain-free through constant monitor every biological function of the patient’s body. Anaesthesiology is inseparable from modern surgery and it is meant to keep patients safe, comfortable and pain-free during the operation, it adds.
The study says that in rural hospitals, anaesthesia is given by unqualified technicians, thus endangering lives of people almost on daily basis. In the process, routine surgeries are turning fatal due to unsafe anaesthesia practices.
Anaesthesia is crucial for pre-operative, intra-operative and post-operative and all hospitals doing surgical practice must have qualified anaesthetists with the designated roles and responsibilities.
It says that HCC should make it mandatory for hospitals to have trained anaesthesia staff. It says that hospitals empanelled under SCP programme must have the services of qualified anaesthesia providers. It adds that HCC must link compliance to patients’ safety to presence of trained staff to re-imbursements made from SCP.
KPSA has asked the government to encourage hospitals to invest in qualified staff and safe practices, promote incentive-based compliance for both private and public healthcare providers. It says that private hospitals should be made accountable for not providing safe anaesthesia services to patients.
It says that HCC should implement its own minimum service delivery standards related to anaesthesia and establish a policy advisory body focused on strengthening anaesthesia services across the province.
The society wants policy reforms for anaesthesia safety and quality, facilitate collaboration among key stakeholders and recommend solutions to systemic challenges to streamline decision-making, enhance inter-departmental coordination, proactive identification and resolution of issues.
The study says that hospitals, especially in private sector, are conducting huge number of major surgeries without qualified or even trained anaesthetists.
It says that SCP is being used in all private hospitals regardless of any presence of anaesthetist and HCC is not doing enough to provide basic right to patients in the form of safe surgical procedures.
It says that HCC should stop the illegal practice through licensing and accreditation and audit mechanisms to improve patients’ safety, standardised practices and reduced risk in peripheral areas.
Published in Dawn, September 16th, 2025