Copyright The Boston Globe
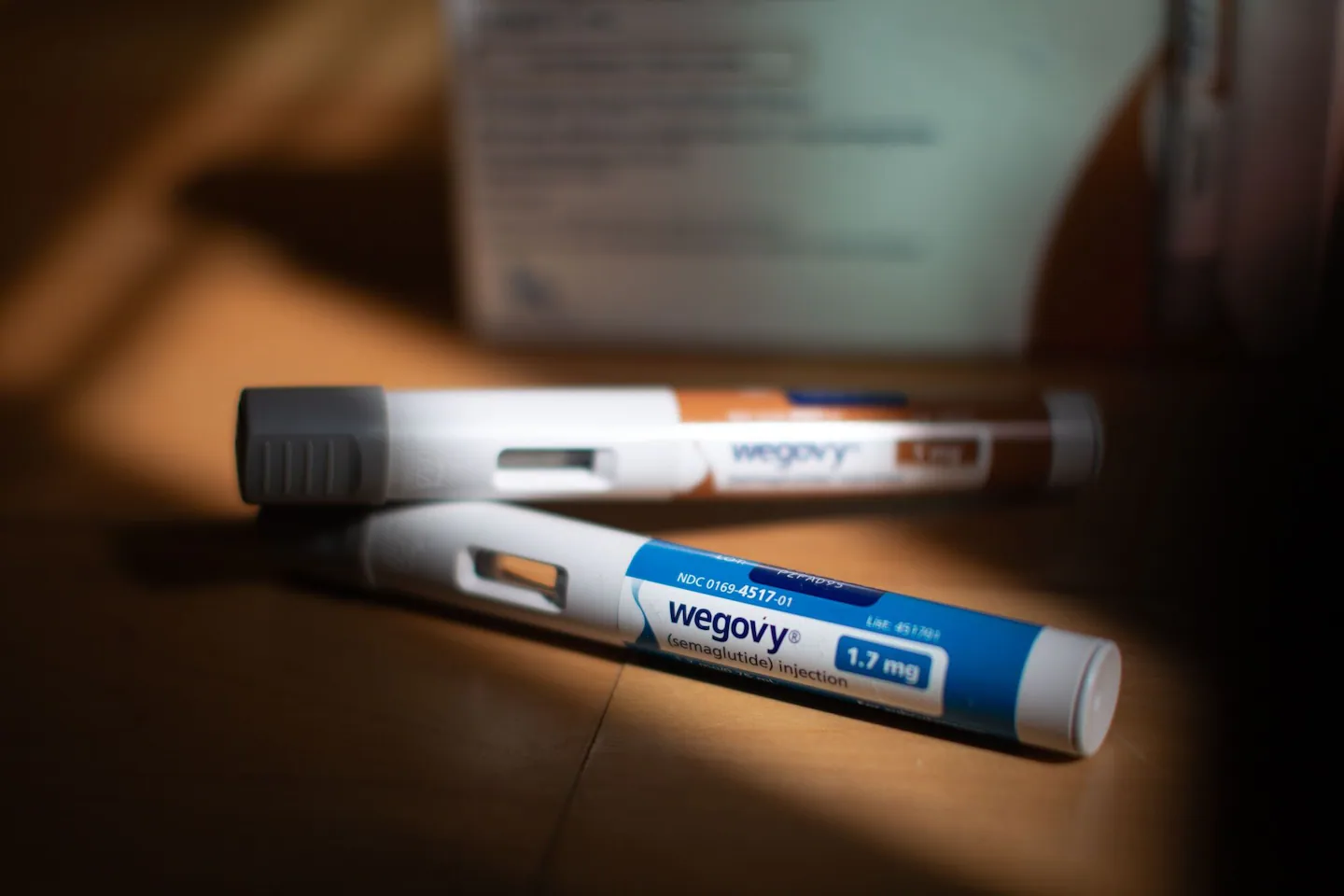
GLP-1 agonists have a crucial role to play in addressing obesity and reducing morbidity and mortality. Although their long-term side effects aren’t fully understood, studies to-date show they are safe and effective for use, and that their health benefits generally outweigh their side effects for most people. There hasn’t been a breakthrough in medications with such tremendous public health relevance related to chronic disease prevention since the advent of statins in 1986, which revolutionized treatment of high cholesterol, and protease inhibitors in 1996, which turned HIV from a death sentence to a chronic, manageable illness. The effectiveness of GLP-1s has made them increasingly popular. Nearly half of primary care patients we see at Open Door Health ask about GLP-1s. Twelve percent of Americans report having taken them. Yet despite the incredible efficacy of these medications, they are becoming less accessible. Health insurance companies are changing their policies to continue covering GLP-1s for diabetes but discontinue coverage for weight loss. This is an effort to save costs — these medications can cost more than $1,300 per month, and their widespread use is a major contributor to rising health premium costs nationwide and in Rhode Island. Between 2021 and 2023, commercial insurance carriers in Rhode Island spent over $120 million on GLP-1 medications alone. The Office of the Health Commissioner recently approved an approximate 20 percent increase in commercial insurance rates, and Rhode Island Medicaid announced potential plans to stop covering obesity medications. This leaves many patients having to pay out-of-pocket. Our obesity crisis has worsened in recent years, and most studies based on dietary changes alone or dietary changes with exercise demonstrate that patients achieve and sustain far less weight loss compared to patients who take GLP-1 angonists. Let’s be clear: restricting insurance coverage for GLP-1 medications is not a data-driven population health strategy, it’s a strategy for controlling costs. It’s time to follow the science and prioritize a new population health strategy. We should be adopting strategies that incorporate the medications in tandem with healthy eating and exercise programs. To make GLP-1s more accessible, we need bold new policies that shift the paradigm for controlling costs by moving from a high-margin, low-volume drug sales model to a high-volume, low-profit margin model. The first common sense way to approach this is through bulk purchasing agreements, which allow organizations to buy large quantities of medications in exchange for lower prices. Although Rhode Island is small and doesn’t have a large market share for price negotiations, our state Medicaid offices could join consortiums for bulk purchasing these medications with other states that have more purchasing power. An additional step is implementing cost controls on drug prices, an approach used in Europe and every other industrialized country. While many policymakers are loath to adopt price controls for fear of alienating the influential pharmaceutical lobby, if there’s a time to adopt price controls, it’s now. GLP-1s may not be a panacea for our obesity crisis. We don’t yet fully understand the long-term side effects, or how best to sustain weight loss over time. We also still need to figure out how to get more Rhode Islanders to change their diet and be more physically active. Over half of patients stop taking GLP-1s, often because insurers stop covering them when people achieve their weight loss goals, they can’t afford out-of-pocket costs, or because they experience gastroenterological side effects. When they do, their weight often rebounds. What’s the bottom line on this issue, scientifically? The science shows that ALL interventions, including GLP-1 agonists, diet and active living, need to be sustained over time. Lifestyle changes become increasingly important to sustain weight loss, particularly if people stop taking medications. However, GLP-1s are true game-changers in the fight against obesity. While they may initially be expensive, costs will come down over time with price negotiations, and as the business model evolves and more products are introduced. We need a public health solution for a nationwide obesity crisis that affects far too many people in our state. Limiting access to medications for patients who need them is not the answer. We need to take the long view and think more strategically and realistically about the crucial role of these medications in contributing to the health and well-being of Rhode Islanders.



